Background
Advances in diagnostic methods have enabled the detection of cancer at the earliest stages when the chances for successful intervention are highest. For many solid tumors, the best chance for a cure is surgery. A surgical cure depends upon the complete removal of all cancer tissue from a patient (a “complete resection”). The main challenge of this approach is that it is very difficult for a surgeon to determine where diseased tissue ends and healthy tissue begins. The result is that many surgical resections fail to remove all cancer, requiring the patient to undergo additional procedures and treatments, with associated risks and potentially poor outcomes.
Existing Solutions
The current, “gold-standard” approach is post-procedure pathology. Pathological examination of surgically-removed tissue usually occurs some days after the procedure. A very small percentage of the removed tissue is subjected to evaluation and sampling errors lead to significant false negative results. A positive finding in pathology requires the patient to return to the hospital for additional surgery or other treatment procedures.
Depending upon cancer type, several interoperative methods may be used (for example, touch prep or frozen section, among others), but each has significant disadvantages. There is a clear, unmet, clinical need for a method to assess the status of marginal tissues around the main mass of a tumor during surgery, enabling complete resection in a single procedure.
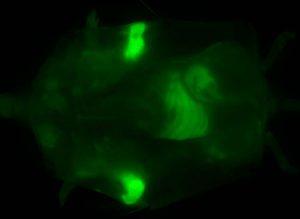
Molecular probes are a promising approach that has the capability of meeting this need. In many cases, these probes target a cancer-associated protein and bind to it. They carry a glowing fluorophore that, in some cases, can be seen visually; however, many probes use near-infrared wavelengths that are invisible to the eye and require an imaging system tuned to detect the glow. But these probes also have significant problems, among them:
- Most require the IV administration of pharmacologically-significant amounts of probe hours, or days before surgery. They build up gradually in the tumor until the fluorescent signal is detectable
- They are “always on,” so the fluorophore glows at all times. Surgeons must deal with significant background glow as they examine the tumor
- Because large amounts of probe are required, they must negotiate the same long and expensive regulatory path as new drugs
- They cannot detect small tumors, or areas of tumor that do not have circulating blood supply (vasculature)
- Because most of these probes target tumor proteins, they “light up” the whole tumor, producing a signal that may swamp signal from marginal tissue, making the precise identification of the tumor margin problematic.
Akrotome FIRE™ – a Better Solution
We designed our FIRE probes to address these problems
- FIRE is applied directly into the surgical cavity topically
- Only minute amounts of probe are used, so the regulatory path is less complex, shorter, and significantly less expensive
- FIRE activates in as little as 2 minutes
- FIRE targets cancer-related enzymes that are more concentrated in tumor margins, enabling the extent of diseased tissue to be precisely imaged
- FIRE is a quenched probe—it activates only if it binds to active cathepsins, so there is virtually no background signal
- FIRE can detect non-vascularized tumors and metastases
FIRE provides a superior solution for the intraoperative visualization of cancer margins for guided surgery applications. FIRE’s high sensitivity and specificity, coupled with its likely simplified approval path, offers the potential for superior ROI in an abbreviated time frame.
To learn more about investment opportunities for FIRE, please click here to email your inquiry. We will respond within one business day.
FIRE from Akrotome Imaging – guiding surgeons to a surgical cure for cancer
- About Akrotome
- More about FIRE
- The technology behind FIRE